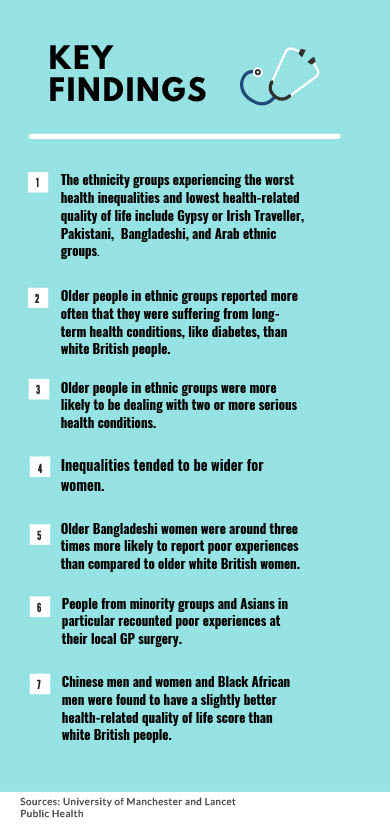
Ethnic minorities are being let down by the NHS, according to a University of Manchester study, as findings reveal wide health inequalities between minority groups and white British people.
In some groups the impact this has is so profound that their overall health is equivalent to the health of someone 20 years older.
People from these groups are also more likely to report insufficient support from local services to manage long-term health conditions, lower confidence in their abilities to manage their health and poor experiences at their GP.
Health-related quality of life is worse for 15 out of 17 ethnic groups compared to white British people, many of whom are living in poverty, the study found.
Some 60-year-olds belonging to Gypsy or Irish Traveller, Bangladeshi, Pakistani and Arab groups were also found to have health similar to the average 80-year-old.
Authors of the research, published in Lancet Public Health yesterday, have said prejudice within the NHS may be exacerbating these health inequalities amongst some minority groups.
Lead author Dr Ruth Watkinson from The University of Manchester said: “This suggests the NHS as an institution is failing people from some ethnic groups.
“Policy action is needed to transform healthcare and wider support services to make sure they meet the needs of all individuals in England’s multi-ethnic population fairly.
“But policy makers also need to address the structural racism that makes it harder for people belonging to ethnic minority groups to access socioeconomic opportunities because poverty is a major cause of poor health.”
Researchers used GP Patient Survey, a programme used to monitor the quality of NHS services and for patient feedback, to collect data.
A sample of 150,000 out of 1.4 million GP Patient Survey responses were used, making it England’s most extensive ever study of ethnic minority health in the over-55’s.
Co-author Dr Alex Turner, also from The University of Manchester, added: “Researchers haven’t been able to research the health outcomes of people over 55 in ethnic minority groups, because they aren’t included in sufficient numbers in most datasets.
“And much official data doesn’t distinguish between groups, which can mask inequalities.
“But this study allowed us to analyse results for all 18 of the UK census ethnic groups separately, allowing us to see differences between them.
“However more research to better understand exactly what drives these health inequalities. There needs to be more data collection with much better inclusion of people from ethnic minority groups in longitudinal studies.”
It’s thought that the study can provide some insight into the high numbers of COVID-19 deaths amongst minority groups.
An NHS spokesperson told MM: “While of course the determinants of health and wellbeing stretch far beyond health care itself – and include jobs, housing, income, diet, exercise and wider social inequalities – the health service also has a key role to play in supporting diverse communities to stay healthy and access high quality care.”
Main photo by Hush Naidoo on Unsplash



