“It took years of being called hysterical to get my diagnosis and I’m still not getting the support I need to live my life the way I want.”
Leila Martyn is a mother of two in her early forties. She was diagnosed with PCOS as a teenager and was told she would struggle to conceive.
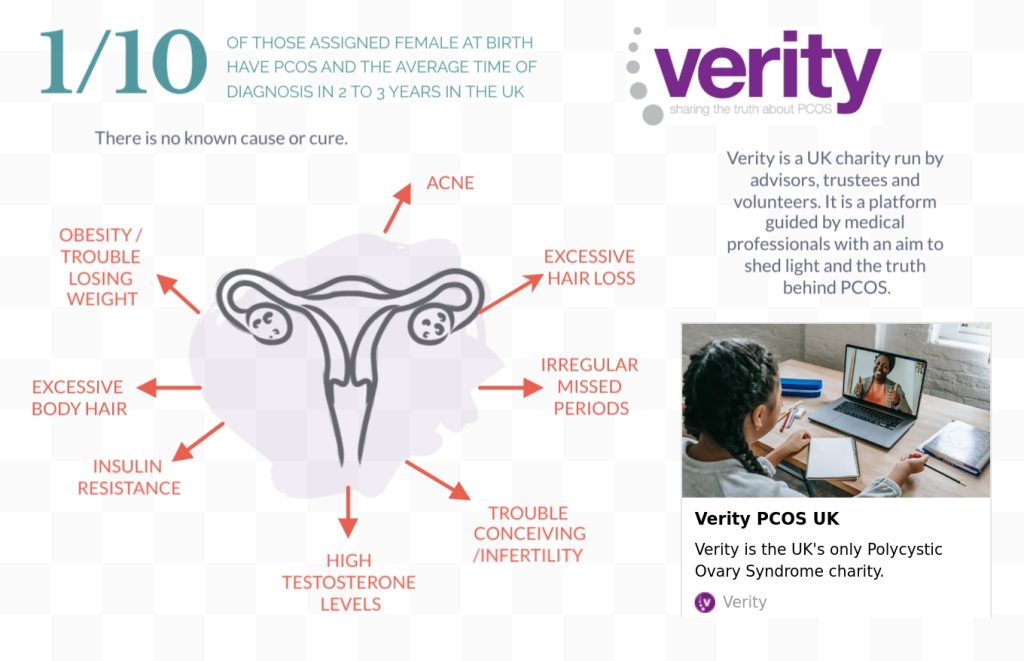
The NHS defines polycystic ovary syndrome (PCOS) as a common condition that affects how a woman’s ovaries work.
There is currently no known cause or cure.
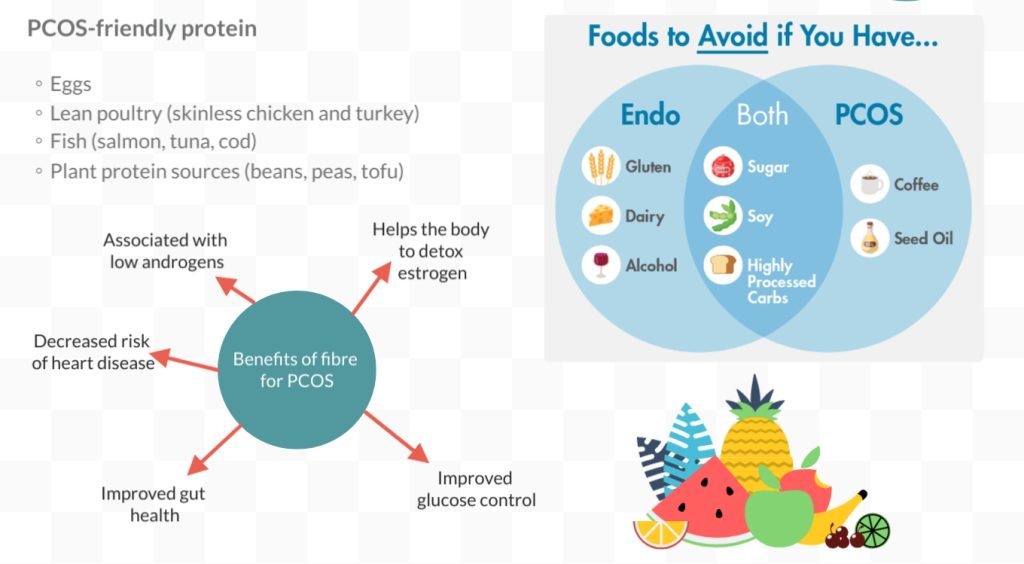
After her fourth miscarriage, Leila began to research recurrent miscarriages in relation to PCOS and discovered that it causes low egg quality. Determined to find a solution, she came across a natural food supplement, Myo-inositol.
There were promising studies supporting its effectiveness in treating many symptoms of PCOS. Leila felt the benefits within a few months of taking it, sparking the idea for her brand MyOva which Leila launched in 2016.

Leila said: “Knowledge undeniably empowers women when it comes to their health and this rings true for PCOS.
“I grew to understand the immense importance of self-advocacy. It became clear to me just how vital it is to equip women with the education about PCOS, enabling them not only to pursue a diagnosis but also to make well-informed decisions regarding their overall wellbeing.”

In September 2022, MyOva launched a government petition to include PCOS and Endometriosis in the national secondary curriculum which ran until March 2023.
Leila also provides an online community for discussion and sharing experiences called The PCOS Collective.
Thousands of women are affected and wait years, including Agatha who after 18 years of dealing with PCOS is finally receiving a remedy to alleviate some of the symptoms.
I’ve asked for 18 years ever since I was diagnosed with PCOS to be put on this as part of hormone therapy. I cried my eyes out yesterday when the I saw that the dermatology department included that in my prescription orders. I can’t believe I might actually find some relief.
— Agatha Snarkness (@rockcandy87) May 24, 2023
Amy, Megan and Courtney
Laila is just one advocate for PCOS in the UK supporting young people who are faced with its challenges and uncertainties.
For Amy, it took seven years to get her diagnosis after a few ultrasounds came back as inconclusive.
Amy said: “They didn’t want to diagnose me because I was a teenager and my hormones were all over the place but I knew something was wrong.”
She continues: “I finally got a blood test that conclusively showed the high testosterone level and it was an immediate diagnosis at that point. My final doctor really advocated for and believed in me, perhaps because he was young. But it’s been years of fighting to get here, years of being told I’m hysterical. And now I have to face the fact that I’ll always have this.”
When Megan’s blood test showed high testosterone – just like Amy’s did – a male nurse advised her to back onto the pill. But she felt this was just masking the symptoms and she declined.
She said: “It can be really tough to deal with when you don’t know what’s affecting you.”
For Courtney, her primary symptoms of PCOS include weight gain, facial hair gain and loss of hair.
Courtney said: “I remember vividly one night I woke up with excruciating pains in my lower stomach to the point where I couldn’t move and I was physically sick.
“I was booked into a pelvic exam and an ultrasound and blood tests, and after a few weeks, I received the news over the phone. It was a bittersweet moment as I was happy I finally had a diagnosis.
“But also getting told that there is a chance I could be infertile was devastating.
“I have found ways to cope with the pain. However, from time to time the pain will still be severe and as I have asthma I can only take paracetamol.”

What have studies shown?
PCOS affects one in ten of those assigned females at birth, and yet the average diagnosis time is between two to three years due to a lack of funding and resources.
Numerous studies have shown a high risk of developing other illnesses such as diabetes and abnormally high blood pressure.
A study published by the Archies of Medical Science explored the relationship between PCOS and Covid-19.
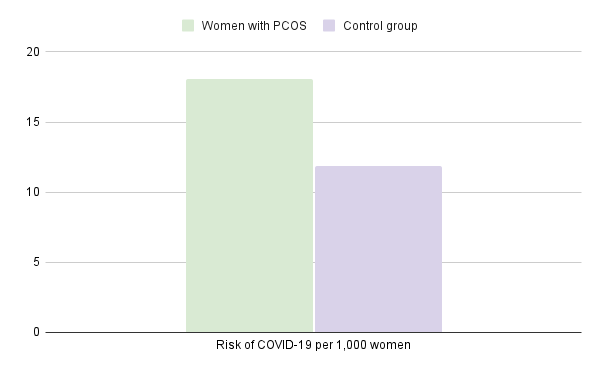
Incidences of COVID-19 in women with PCOS were almost twice the rate than in women without PCOS; 18.1 cases per 1,000 person-years compared to 11.9 cases without PCOS).
Co-author of the Royal College of Surgeons of Ireland Dr Michael O’Reilly said: “Before the onset of the COVID-19 pandemic, women with PCOS consistently report fragmented care, delayed diagnosis and a perception of poor clinician understanding of their condition.
Women suffering from this condition may fear, with some degree of justification, that an enhanced risk of COVID-19 infection will further compromise timely access to healthcare and serve to increase the sense of disenfranchisement currently experienced by many patients.”
Eilidh, 23, from Glasgow qualified to become a midwife in 2022. She developed PCOS symptoms during the pandemic after withdrawing from oral contraception.
In a new podcast episode, Eilidh discusses her diagnosis and experience, as well as the lack of awareness and funding that goes into research for female reproductive health.
She said: “I remember having to leave school early or just not go to school at all.
“You just feel like it’s not a good enough excuse to call in sick.”
Eilidh continues: “Now doing the job I do, I see how common it is.
“In my job people are pregnant and so it’s like oh there are no fertility issues but you can see ‘Oh, she’s got PCOS’ and so in terms of the everyday symptoms I think we still have a long way to go.”
Verity is the only UK PCOS charity within the UK which supports the community by presenting the truth behind the diagnosis.
PCOS advocate Jo Bratton said: “The GP did a scan and told me everything was “pretty much normal” and not to worry. 10 years later, I was diagnosed with PCOS and possible endometriosis.
“However, wasn’t to make a deal of it unless I was trying to get pregnant.”
Fia also identifies the stigma associated with PCOS and fertility and suggests the focus is primarily on the difficulty to conceive when discussing the challenges PCOS presents.
They said: “I don’t think there’s enough awareness of PCOS. When it is spoken about, issues around fertility are the priority and it’s only really cis women in their 30s talking about it because they’re dealing with fertility issues.
There is no mention of the struggles with irregular periods, increased body weight and excessive body hair, and the self-esteem issues that come along with that.”
According to the PCOS Awareness Association 27-50% of those with PCOS experience high levels of depression and anxiety.
If you are seeking support or advice, visit Verity support here.




