From the pill to the implant, long-acting contraception has always been a female responsibility. But with the first-ever trial of a non-hormonal male pill ending next month, could men soon share the burden?
It was my third year of university. The year I spent wild swimming in the river, drinking cheap wine on bedroom floors and studying for my final exams.
It was also the year I started taking the pill.
My boyfriend at the time suggested I go on the medication. I’d heard the horrors from friends, the depressive thoughts, the anxiety, the pimply faces and the weight gain. I told him I didn’t want to but – with a 99% success rate in preventing pregnancy – it seemed like a no-brainer.
So why did contraception feel like a burden? It was because as a woman who was in a heterosexual monogamous relationship, the duty of contraception was wholly down to me.
Long-acting highly-effective contraception, like the female pill, UID, the patch and the implant, all worked in female bodies.
I asked my boyfriend, ‘If there was a male equivalent to the pill would he take it instead of me?’ He said ‘yes’, but with no option on the market at the time, he didn’t have to confront that reality.
But with the first human trial of a hormone-free male pill ending next month, and a long-acting contraceptive gel trialled last year, all of that could change.
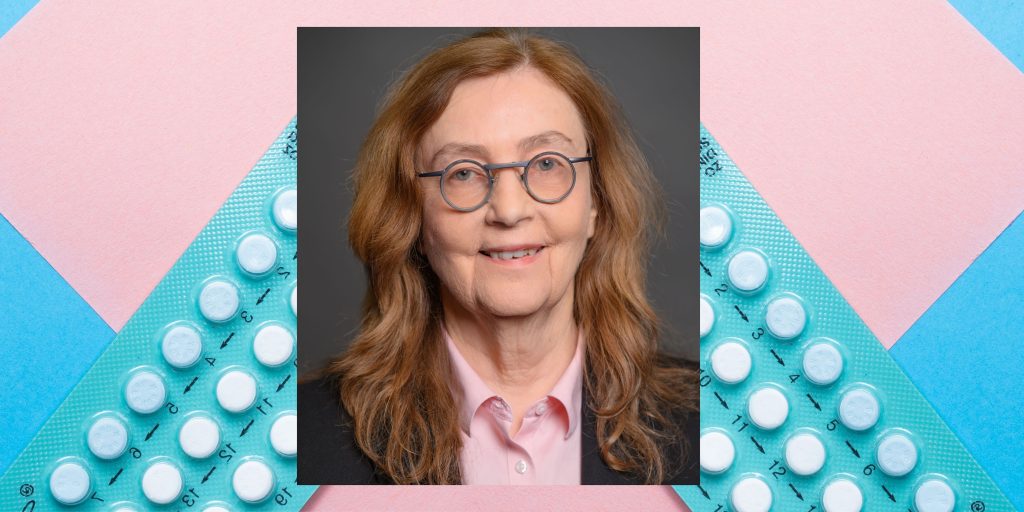
“The last innovation in contraception was the birth control pill for women, and that’s more than 60 years ago,” said Gunda George, a co-creator of YCT-529, the non-hormonal male pill.
“The world is ready for a male contraceptive agent.”
YCT-529, developed by the University of Minnesota, was found to be as successful at preventing pregnancy as the female pill in preclinical trials.
Credit: Gunda Georg and Unsplashed
It works by blocking sperm production using vitamin A and is “99% effective and 100% reversible with no side effects” according to YourChoice Therapeutics, its manufacturer.
Until now, men could either use condoms, which are reversible but only 82% effective with typical use according to the NHS, or get a vasectomy, which is a permanent procedure.
George, professor of medicinal chemistry at the university, said delivering a pill “that’s hormone-free is simply the right thing to do given what we know about the side effects women have endured for decades from the pill”.
YCT-529 is now being tested for its safety and tolerability in 16 British men in a Nottingham-based trial run by the pharmaceutical firm Quotient Sciences.
Due to finish in June, Georg – who has been developing YCT-529 for over 15 years – said: “I have not heard anything but good news so far. There are no unwanted side effects in any of the men as far as I have heard.”
She hopes that after the full evaluation of the pill, bigger trials – which eventually use couples – can begin, with the pill available to buy within the next five to six years.
While she acknowledges the long wait, she notes her pill is not the only contraceptive in development. She said: “Ours is the first non-hormonal contraceptive to come to clinical trial. But come to think of it, there is the hormonal gel also in clinical trial and it is quite promising that the whole field is moving forward.”

Credit: © Regents of the University of California, Davis. All rights reserved. The photographer is Karin Higgins
A long-acting reversible hormonal gel has also been tested in men in the US, Kenya, Chile and the UK — and Matthew Treviño and his partner Emily Fletcher were part of that trial.
The couple from Sacramento, who are in a long-term monogamous heterosexual relationship, a prerequisite of the study, signed up to trial Nestorone at UC Davis in California.
Treviño, 35, was interested in finding a less invasive alternative to a vasectomy and in taking some responsibility in preventing pregnancy, as Fletcher, 28, had been on contraception for the past 15 years.
Treviño said: “I don’t think it is fair that a woman can get pregnant once or twice a year, while a man can get a woman pregnant everyday, even multiple times a day if it’s multiple women.
“I always thought the onus was on the wrong side there.”
Treviño, who is also a researcher at UC Davis, started applying the gel once a day to his chest from August 2022.

The gel, which contains segesterone acetate, a synthetic progestin which is also used in female contraceptive pills, blocks the male sex hormone testosterone, and prevents sperm production. The gel also contains replacement testosterone to help maintain sex drive and normal function.
After three months,Treviño’s sperm count dropped to zero and Fletcher had her IUD removed – the gel was the only form of contraception for the couple the following year.
He added: “Once we got past the first couple of months, and seeing her body adjust to not being on contraception, and seeing the minimal side effects that I was experiencing, we were 100% on board. We were trying to extend our time on the study because it was great, I had no issue.”
Treviño said the “experience had a very minimal impact on my life”, noting weight gain, increased libido (“not a bad thing”, he joked) and acne on his chest as the only side effects. However, like the female pill, the list of potential side effects is long, and men could also experience changes to mood, hair condition, skin condition, decreased libido and insomnia.
Treviño said he would recommend the gel to any man and already said he had colleagues who were interested.
However, only 52% of 2,021 British men said that they would take the male contraceptive pill, according to the most recent study by the Independent Pharmacy in 2022.
Professor Katrina Kimport, who researches gender, reproduction and health at the University of California, argued that it is not only the lack of male alternatives, but narrative around contraception, which is making the responsibility “largely feminised”.
Kimport, author of More than a Physical Burden: Women’s Emotional and Mental Work in Preventing Pregnancy, said: “[In heterosexual relationships] some logic that people have is that women care more because it is in their bodies. Well when you have millions of people who do not want to be pregnant, it baffles my mind that every single woman would want it more than every single male partner.”
She also pointed out that medical care systems “only serve people with the capacity for pregnancy” instead of a couple-based approach to contraception, which she recommends.
She said: “Since it is women who are going to these clinicians in the first place … from the clinicians perspective, if they want to help their patient avoid pregnancy, they are going to burden the hand.
“I have you in front of me and I am going to get you something that would be really effective and prevent pregnancy and although there are other things that don’t require you to take on that responsibility, I don’t have your partner in front of me.”
About a million more women than men accessed sexual health services in England, according to 2022 data from the UK Health Security Agency, highlighting women are more likely to take initiative when it comes to their reproductive health.
However, when male contraception becomes a reality, these figures could soon change.
Georg already noted increased interest in her trial, with her research group receiving emails from several men wanting to participate. And alongside a changing attitude towards contraceptive responsibility, men could soon share the contraceptive burden.
Trevino said: “It is definitely a couple’s decision. I take her [Fletcher] health into account just as much as I take my own. Knowing how well she did off birth control, and how little it affected me, it’s like why not just continue with this.”
He added with a smile: “I’m doing this for you ladies.”