Guidelines say everyone should be offered anaesthetic for coil fittings but only two in three patients were last year, new data reveals.
The national benchmarking audit, published by the Faculty of Sexual and Reproductive Health’s (FSRH) clinical effectiveness unit, revealed that – on average – services made two in three patients aware of anaesthetic options at coil appointments.
Based on new FSRH guidelines, all individuals should be told about available analgesia (anaesthetic) options for coil insertions, and referred elsewhere if what they want isn’t available.
While a quarter of services did achieve this standard, almost 11% of services didn’t offer any patients anaesthetic, according to the data.
It comes after growing awareness that pain relief is even an option for this procedure.
Dr Francis Yarlett is an NHS GP and medical director at contraception review platform The Lowdown.
She said: “In recent years, one big discussion has been about the coil fitting procedure and pain. When it first started, a load of women decided to cancel their appointments and not have the coil fitted, which is really sad.”
In 2021, BBC presenter and journalist Naga Munchetty shared her “traumatic” coil fitting experience during a BBC 5 Live programme.
Munchetty found the procedure excruciating but acknowledged many women “have no problem at all”. The issue, she said, was not the coil itself but about how we look at women’s health and pain more broadly.
Dr Rebecca Strauss, clinical director of FSRH’s CEU, said: “Women should be given the option of analgesia, and clinicians who insert intrauterine devices are encouraged to look at the FSRH guidance.”
The audit, published earlier this year, includes data from 64 services, including 53 from specialist services like sexual health clinics and hospitals, and 11 from GPs.
FSRH said some of the audit’s figures may be due to a lack of documentation.
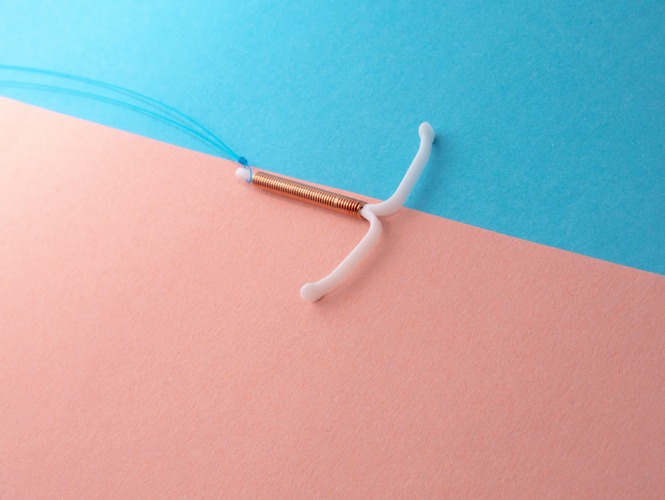
What is a coil?
A coil is a small t-shaped device inserted into the womb through the cervix using a speculum to open the vagina. There are two types of coils – an IUD, or copper coil, which prevents pregnancy by releasing copper into the womb, and an IUS, or hormonal coil, which prevents pregnancy by releasing the hormone progestogen.
Having the coil, Yarlett said, can be “a really great experience, but it just takes a little bit more persuading now”.
She added that she doesn’t think this is necessarily a bad thing and hopes these conversations lead to more women advocating for themselves for pain relief “so they can get this really good, long-acting, lasts-for-six-years contraceptive”.
There was actually a slight increase in prescriptions for the coil between 2021/2022 and 2022/203 – back up to pre-pandemic levels, according to data from the NHS Business Services Authority.
The insertion “went probably as good as it could” and apart from “a sharp pain when the IUS went in”, Amie said it was over relatively quickly.
She was advised to take some paracetamol beforehand but forgot, and while the clinician checked she was still happy to proceed, no local anaesthetic was offered.
Amie, now based in London, said she had a much more painful experience when her coil was removed last year.
After an unsuccessful “nightmare” attempt at her GP surgery to remove it, Amie booked a hospital appointment, where a gynaecologist had to take it out.
Despite experiencing severe stress and pain, she wasn’t offered anaesthetic at any point during the appointments, and said: “I planned to get a new one in pretty quickly, but it’s been nearly a year now, and I’m more nervous about a new one than ever.”
There are three main local anaesthetic options: a paracervical block (injection), an anaesthetic spray, and gels and creams.
The 10% lidocaine spray significantly reduced insertion-related pain scores compared to placebo, in this randomised control trial, and the spray was more effective than lidocaine injection and cream, according to this 2017 study
There’s no scientific evidence for the preventative use of ibuprofen, according to a statement published by FSRH.
Yarlett said the local anaesthetic spray is a good option because it’s cheap and the bottles are reusable, whereas administering anaesthetic injections requires more training, which, in turn, requires more resources.
English council spending on sexual health services has been cut by more than a third since 2013, according to a recent Guardian analysis.
Although not all women will want anaesthetic and may manage well with ‘vocal local’ — “a well-trained healthcare assistant to chat to them through the procedure” — Strauss said women should ideally always have the option.
Lucy Rodd, 25, got a coil earlier this year and was advised to take paracetamol/ibuprofen beforehand. “Analgesia gel was given as an automatic,” she said, and the clinician also “explained exactly what she was going to use and how it would be inserted”.
Lucy added: “The clinic room was a literal cupboard, and the procedure was still painful, but at least I know I was given all the options to minimise the pain.”
Leila Hooton, 25, has had the copper coil inserted three times, most recently two years ago. On the first two occasions, she was advised to take it easy after the procedure and to have some painkillers.
However, she said: “The third time, I was told the nurse was going to apply some anaesthetic jelly, which surprised me because I didn’t know it was a thing.”
She added: “It made the actual procedure so much less painful than the first two times.”
While it’s important to improve awareness of and access to pain relief, FSRH said it’s vital we remember the benefits IUC provides.
Rather than being put off these methods, it encouraged women to discuss anaesthetic options with their clinicians.
Featured Image: Photo by Reproductive Health Supplies Coalition on Unsplash