Surgeons are turning to 3d printing technology to help deal with difficult and complex procedures where normal approaches can have limited success. MM spoke to a team of clinical engineers at Salford Royal Hospital to find out more about the growing use of 3d printing in medical settings – and hear what the future might hold.
A vital first step before many surgical procedures is for a patient to be intubated, involving a tube being inserted into the airway to make sure oxygen still reaches the lungs during surgery.
But patients with complex airways can make intubation almost impossible for even the most skilled clinicians.
And this is exactly what a surgical team at the Liverpool Heart and Chest Hospital encountered recently during one particularly tricky situation.
The team had been forced to cancel a planned surgery for a patient whose airway was so difficult to navigate attempts to intubate them had twice failed.
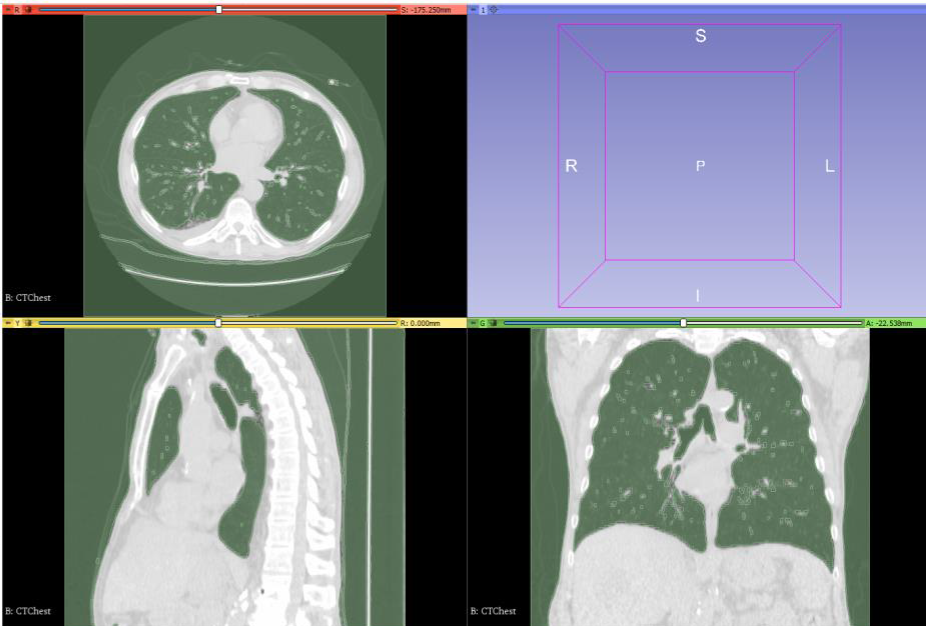
Access to the lungs was restricted by an S-shaped curve somewhere along the airway and the surgeons were unable to see where exactly it was or in which direction it was heading.
“They were in the dark, just prodding about trying to find it,” Stuart Watson said, the head of the 3d Surgical Planning and Innovation (3dSPIN) centre at Salford Royal Hospital.
The surgical team in Liverpool called on the 3dSPIN centre to help them find an alternative approach for safely intubating the patient.
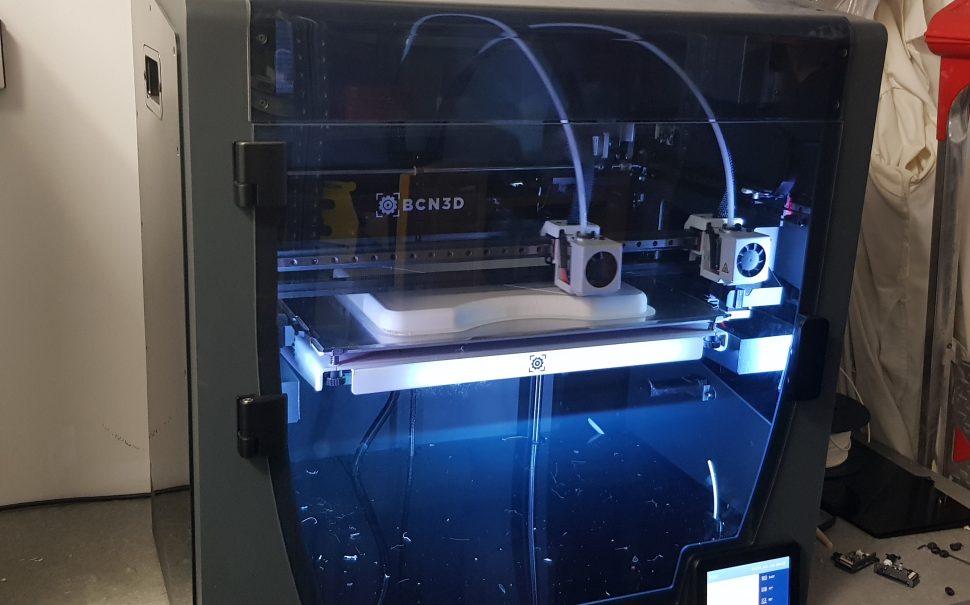
Luckily, the centre had a range of tools built using 3d printing and scanning to support surgical teams with patients exactly like these.
These tools made up what the centre calls a ‘difficult airways package’ and it included a virtual model of the patient’s airway created from CT scan data. The model allowed the team to carry out a ‘virtual endoscopy,’ using the virtual model to explore the airway and see how it could be safely manoeuvred during intubation.
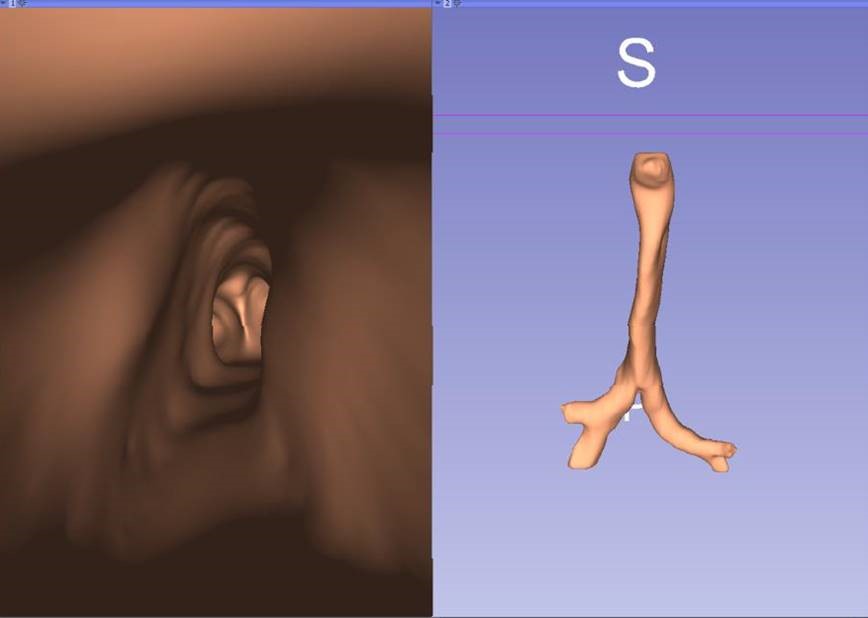
The centre also printed them a physical model made to scale of the airway from a silicone mould and embedded it with foam.
“The silicone gave the same tactile sensation as a trachea,” Stuart said. “And the foam gave it the same consistency as the surrounding muscle and fat tissue – it gave the surgeons the same ‘feel’.”
The intubation was practised on the physical mould until the team felt able to safely navigate the patient’s actual airway.
After practise and preparation, the intubation was performed successfully.
And then – finally – the operation was able to go ahead.
This is just one of more than 50 surgical projects the 3dSPIN centre has carried out since it launched in April 2022. Using 3d printing technology, the centre has been solving complex challenges across the fields of anaesthetics, ear nose and throat (ENT) and orthopaedics.
Its main focus has been to support surgical planning for patients with complex airways – airways which have become restricted or tortuous. And its creation of the difficult airways package has been so successful its use has become routine within Salford Royal.
“Our ENT surgeons and anaesthetists will not perform a procedure without them now,” Stuart said. “They are proven to be necessary and worth the time and effort.”
The difficult airways package is quickly accessible to clinicians. An engineer can create the entire package within three to four hours and the virtual endoscopies can be carried out by clinicians on their mobile phones – and even on a virtual reality headset.
Although such tools might appear to be unusual, their creation has always been driven by the needs of those who request the centre’s help.
This is why the centre began its ongoing collaboration with researchers at the University of Manchester to develop a prototype helmet for stroke triage. It is being built to be able to quickly assess the progress and condition of suspected strokes in a patient by taking rapid measurements of fluid properties in the brain.
Shijie Liang is one of the clinical scientists at 3dSPIN working on this project. She plans to carry out tests this year using the device on patients and volunteers to measure its effectiveness for detection compared to CT and MRI scans.
Shijie said: “Hopefully, we will have some good results and in the future it could be used as a portable detector for strokes.
“Maybe they could be put inside ambulances, or near the bedsides of patients.”
This way, the condition of a patient could be quickly tested in cases where rapid treatment might be needed and there would be no need to wait for the results of scans.
In the years ahead, Stuart expects to see the development of 3d printing in medical settings advance to higher levels.
The technology is already well established for creating anatomical models, such as bone structures and airways, and it is becoming increasingly sophisticated at providing patient-specific instruments and implants.
But at its most advanced, Stuart sees 3d printers being able to produce bio-functional implants, such as soft tissue and organs.
This advancement is also anticipated by Norbert Radacsi at the University of Edinburgh who has been using 3d printing to support kidney cancer patients for the past few years.
Starting in May 2020, Norbert collaborated with a surgeon at the Western General Hospital in Edinburgh. Norbert provided the surgeon’s patients with 3d models of their kidneys which also showed the cancerous tumours that had grown there.
Patients could use the models to see the extent of the cancer and could better understand the surgical procedure needed to remove it.
“We are still doing this, but now we want to go to the next level,” Norbert said. “We want to bio-print functional kidneys.”
Norbert said kidneys are in the highest demand from patients in need of an organ donation all over the world.
And so, once funding for his proposal is granted, Norbert would look to meet this demand in every hospital and medical centre in need with the technology of 3d printing.
All images courtesy of Northern Care Alliance NHS Foundation Trust